
CSF analysis was repeated with a WBC count of 5/μl OCB were not detected (Pattern I). The patient developed new behavioral disorders, and cognitive functions declined (deterioration of short term memory, problems with word finding). The patient further clinically improved showing a mRS score of 1 at month 15.Īfter approximately three years of clinical remission, a slow worsening of psychiatric symptoms occurred. Anti-NMDAR IgG titers declined with a nadir at month 15 after disease onset (titer 1:80). Seizure occurred one month after disease onset requiring antiepileptic treatment with levetiracetam. The patient was treated with intravenous methylprednisolone (IVMP, 1000 mg on eight consecutive days) and plasmapheresis (PLEX, on four consecutive days), which led to a clinical improvement (sequelae: postencephalitic syndrome, short-term memory disturbances, apathy). Eventually, diagnosis of NMDAR encephalitis was made, according to the diagnostic criteria of Graus et al. A whole-body 18 F-fluoro-2-deoxy-D-glucose (18 F-FDG) positron emission tomography (PET)/CT showed no sign of neoplastic disorder, especially no thymoma.

Ri, Yo, Hu, Ma2, Amphiphysin, CV2 IgG were negative (determined by a commercially available immunoblot ).

Presence of IgG directed to MOG (serum titer 1:40 considered negative) and aquaporin-4 (AQP-4) were excluded by an in-house test as previously described. Laboratory examination by a commercially available cell based assay (Euroimmun, Lübeck, Germany) revealed positive NMDAR IgG in serum and CSF (serum titer 1:2560). Electroencephalography (EEG) showed continuous bilateral slowing without epileptic discharges. The patient was referred to the Medical University of Innsbruck, where a thorough diagnostic work-up was done. Additionally, Computed Tomography (CT) scan and consecutive bacteriological examination of tracheal aspirate identified an atypical pneumonia due to pseudomonas aeruginosa.
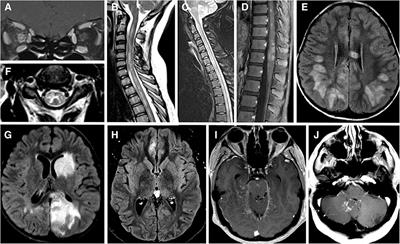
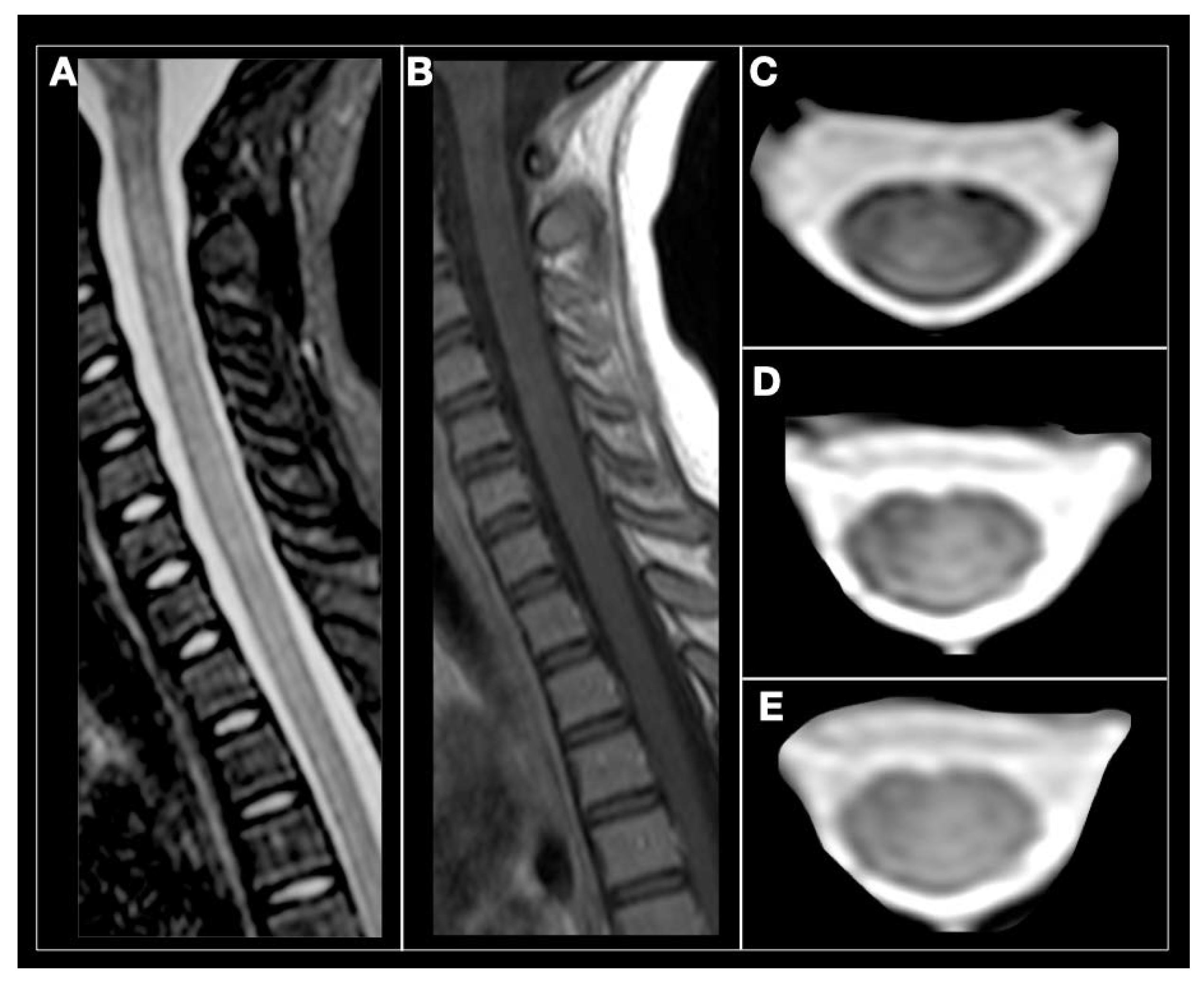
Cerebrospinal fluid (CSF) analysis showed mild pleocytosis with lymphocytes (white blood cell count 38/μl) and CSF-restricted oligoclonal bands (OCB Pattern II). Emergency cerebral magnetic resonance imaging (MRI) revealed a normal scan. Here, we report the case of male patient with anti-NMDAR encephalitis who developed MOG and Caspr2 IgG during the disease course.Ī 32-year old man with a pre-morbid modified Rankin Scale (mRS) score of 0 was referred to primary medical center due to psychosis, behavioral disorders and consecutively movement disorder, decrease in consciousness and hypoventilation. However, none of these reports provided long-term data of the clinical disease course, of antibody titres and radiological findings. either MOG immunoglobulin G (IgG) and demyelinating aspects have been found in patients with anti-NMDAR encephalitis, or vice versa NMDAR IgG in patients with demyelinating CNS disease. Overlap syndromes of these two disease entities have been reported, i.e. Patients with NMDAR encephalitis usually present with a clinical syndrome including psychosis, behavioural changes, amnesia and epileptic seizures, frequently followed by dyskinesia and decreased levels of consciousness, while patients with MOG associated disorders typically present with a demyelinating syndrome reaching from ADEM-like phenotype to isolated syndromes, such as myelitis or optic neuritis. Antibody dynamics were associated with clinical disease course.Īnti-N-methyl-D-aspartate-receptor (NMDAR) encephalitis and Myelin Oligodendrocyte Glycoprotein (MOG) associated disorders are both immune-mediated inflammatory disorders of the central nervous system. We provide long-term longitudinal follow-up of a patient with anti-NMDA receptor encephalitis who developed triple antibody positivity at the time of relapse. Anti-Caspr2 antibodies persisted, anti-NMDA receptor antibodies decreased, while anti-MOG antibodies turned negative again. Treatment with plasmapheresis, steroids and rituximab eventually led to substantial clinical and radiological improvement. At this time, the patient developed anti-MOG and anti-Caspr2 antibodies. Forty-four months after symptom onset and diagnosis of autoimmune encephalitis, he suffered from relapse. We report a 32-year-old male patient who presented with psychosis, decreased consciousness and movement disorders and was tested positive for anti-NMDA receptor antibodies. In this case we provide a long-term longitudinal follow-up of clinical and imaging characteristics as well as of antibody dynamics. Overlap syndromes of anti-NMDA receptor encephalitis and MOG-mediated demyelination have been reported.


 0 kommentar(er)
0 kommentar(er)
